ADHD & Occupational Therapy – Can OT Help Manage ADHD Symptoms?
Was your child recently diagnosed with ADHD? You may be curious about the connection between ADHD & occupational therapy – should you include OT as part of your approach to help your child manage their ADHD symptoms? Whether you choose to use medication or not, working with an OT can be incredibly beneficial. As a parent it is your right to explore all the options & make the best decision for your family, so we thought we’d take the opportunity to tell you a little bit more about OT and how it can help your child
What is occupational therapy?
Occupational Therapy (OT) is a service that provides ages newborn to geriatrics with the skills they need to do the things they love independently! Providers of OT include Occupational Therapists and Occupational Therapy Assistants (commonly referred to as Occupational Therapy Practitioners [OTPs]). They work together to evaluate, create a plan of care, and carry out treatments based on the plan of care and personal goals you or your child may have.
An occupational therapy team can help develop physical skills, emotional skills, social skills, & more. Specifically, for kids diagnosed with ADHD, OTPs can help children build the skills they need to complete daily routines at home such as getting ready in the morning, focus and attend during the school day, and assist with self-regulation for a good night’s sleep.
Common ADHD Symptoms
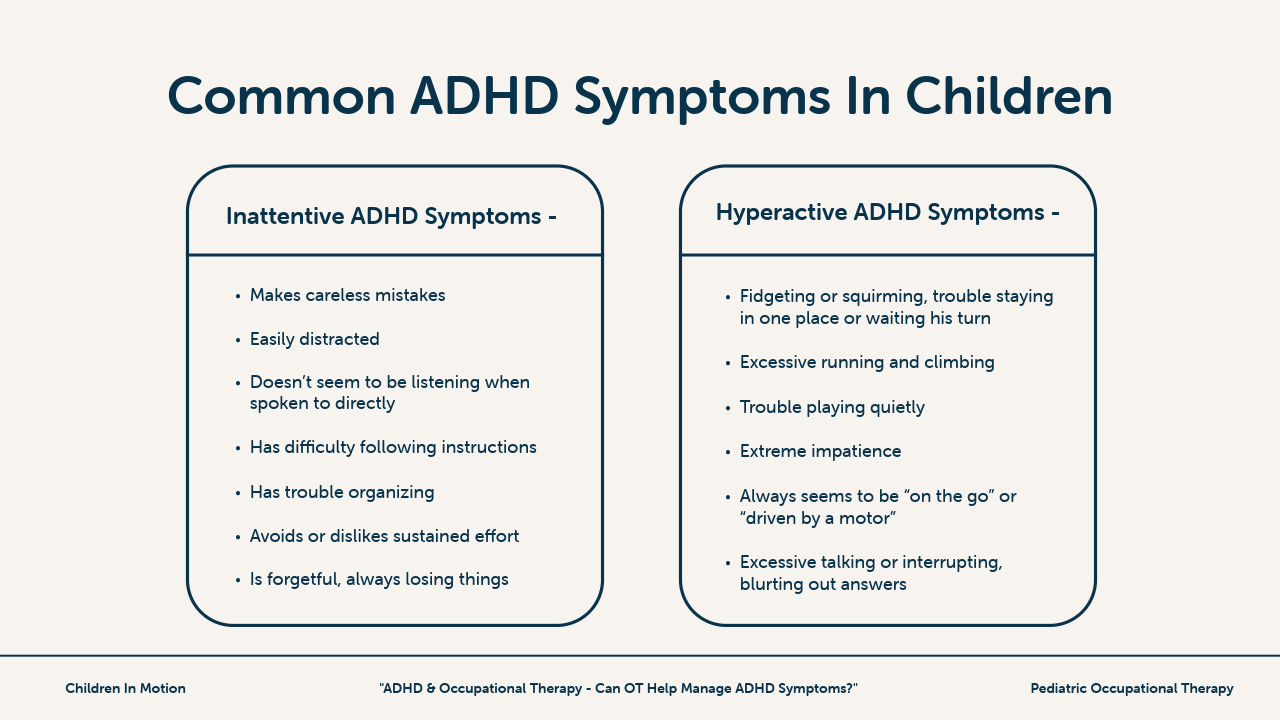
It is important to note there are two different types of ADHD symptoms: inattentive behaviors and hyperactive behaviors.
Inattentive Symptoms of ADHD
- Makes careless mistakes
- Easily distracted
- Doesn’t seem to be listening when spoken to directly
- Has difficulty following instructions
- Has trouble organizing
- Avoids or dislikes sustained effort
- Is forgetful, always losing things
Hyperactive Symptoms of ADHD
- Fidgeting or squirming, trouble staying in one place or waiting their turn
- Excessive running and climbing
- Trouble playing quietly
- Extreme impatience
- Always seems to be “on the go” or “driven by a motor”
- Excessive talking or interrupting, blurting out answers
https://childmind.org/guide/parents-guide-to-adhd/#block_6543e7a86c9d0
An OTP will select activities based on the symptoms your child may be presenting with. There are some cases where a child may have both inattentive and hyperactive behaviors. We tailor activities specifically to the child in occupational therapy, addressing all their needs!
What research says about the effectiveness of occupational therapy for ADHD
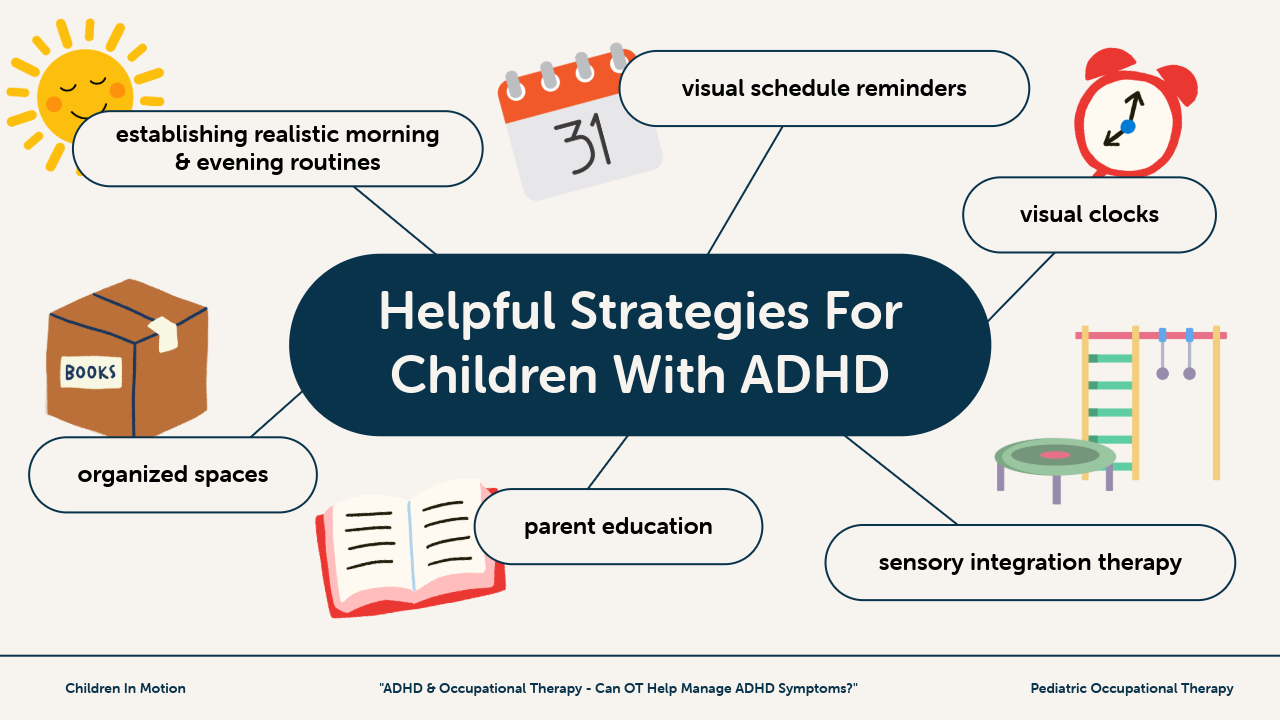
In 2017 a group of researchers took a group of children ages 9 – 15 and evaluated the effect of working with an OT & coach (supervised by an OT) to establish strategies that improve TPA (time processing ability) & DMT (daily time management). This study also examined the effect of providing educational trainings to parents, teachers, and the children about ADHD.
The study took place over 24 weeks, after which significant improvements were identified in time-processing ability (TPA) & daily time management (DTM) when compared to the control group. Some of the strategies that participants in this study used included establishing realistic morning & evening routines, visual schedule reminders, organizing items in a way that make them easy to find, and utilizing visual clocks & timers. (More Information – PMID: 28956183)
Additionally, a common link exists between children diagnosed with ADHD and those facing executive functioning challenges. Executive functioning is essential for organization, planning, task completion, paying attention and more. A group of researchers in China, also in 2017, examined the efficacy of using a cognitive training program as a non-pharmacological treatment for ADHD.
In the study participants worked with an occupational therapist to use visual cues & repetition, paired with providing parent education & coaching. At its conclusion, the study determined these methods greatly increased the executive functioning of participants and can be a viable alternative to ADHD medication. (More Information – PMID: 28229986)
Is Sensory Integration Therapy helpful for ADHD?
Sensory Integration Therapy is a treatment model that focuses on using sensory experiences to adjust the neural pathways in the brain. Jean Ayers established this modality of treatment in the 1970s to help people with sensory processing disorder. Sensory processing is a foundational neural function that affects many areas of our day to day life.
A study conducted in 2014 investigated the sensory processing abilities of children diagnosed with ADHD & found that compared to a control group of children (not diagnosed with ADHD), children with ADHD showed significantly more impairments with sensory processing skills, as well as in their behavioral and emotional responses. (More Information – PMID: 25076000)
In another study in 2016 researchers explored the effect that sensory integration therapy has on children diagnosed with ADHD. The study included 12 therapy sessions, spanning over 6 weeks, during which participants participated in various therapeutic activities that focused on balance, spacial awareness, hand eye coordination, motor coordination, and more. At the conclusion of the study researchers found that sensory integration therapy increased executive functioning by 46.7%. (More Information)
Frequently children diagnosed with ADHD also have challenges with executive functioning, so the improvements noted in this study are very encouraging. Although these studies are helpful & back up what we experience when we use sensory integration therapy with our clients, further research about the benefits & effectiveness of sensory integration therapy is ongoing.
What to expect during an occupational therapy session
Typically treatment sessions are typically 60 minutes in duration. At our clinic, our therapy sessions are child led, meaning that we take the child’s interests & preferences, and work them into the treatment sessions. We approach each session with the child’s specific treatment goals in mind (and usually with a few activities planned), but we also make sure to leave plenty of room to be flexible depending on how the child is feeling that day.
Some of our clients favorite activities include swinging on the sensory swings, creating & completing obstacle courses, and jumping in the ball pit. Incorporating plenty of muscle work & movement throughout the session ensures we maximize the therapy sessions & keep our kiddos grounded. If the child’s parent is able to join us during the session, we also like to take the opportunity to answer any questions they may have and teach them strategies they can use at home. Occupational therapy sessions are meant to be challenging, but also FUN!
How to find an OT (and what to look for)
To start, the medical professional who diagnosed your child should have a referral list that they can share with you. You could also reach out to your pediatrician to see if they have any recommendations. Lastly, another place to look for an OT is with your insurance provider.
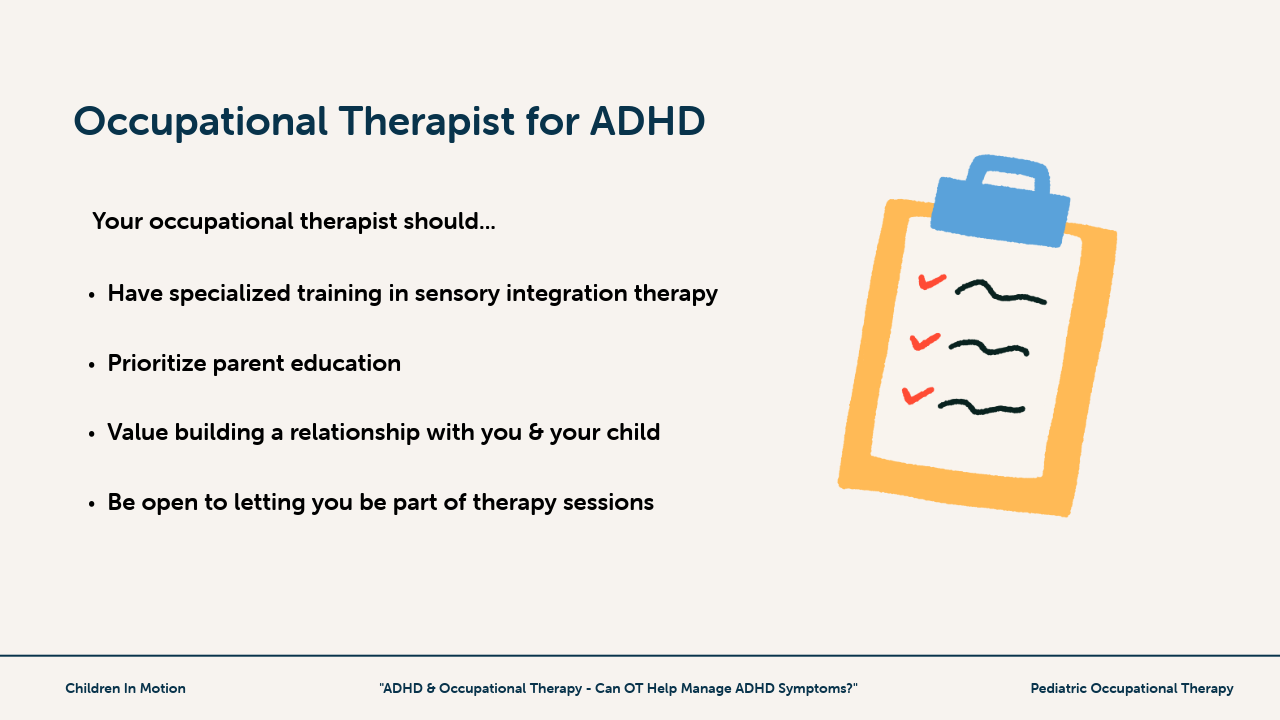
You will want to look for an OT who has specialized training in sensory integration therapy, and who also prioritizes parent education. In order for OT to be beneficial for children managing ADHD symptoms, parent education has to happen. It’s also important that the occupational therapy practitioner builds a connection with you & your child. Don’t be afraid to ask to sit in on sessions, give feedback, and request specific strategies to work on at home. The therapy process should be a collaboration between everyone involved.
In conclusion, yes, occupational therapy can be a viable solution for managing your child’s ADHD symptoms. Whether you choose to pair occupational therapy with medication – or choose one or the other – we encourage you to find what works best for your family & stick to it! There is no right or wrong way to approach this, just what is right for your family. As always, contact us if you have any questions and make sure you check out our blog for more sensory processing, self regulation, & occupational therapy resources!
Want to know more about sensory processing, self regulation, child development, & more? Our resource library is full of free crash courses, guides, and tools to help you understand more about your child & how you can support them outside of therapy.
Get your free resources!
show me the resources